Blinatumomab in relapsed acute lymphoblastic leukaemia
This honours project will investigate resistance mechanisms to the bispecific T-cell engager (BiTE) blinatumomab in relapsed acute lymphoblastic leukaemia.
Recently, a new compound of drug known as Bispecific T-cell engager (BiTE) has been approved for use in B-ALL by the Food and Drug Administration (FDA) and is currently undergoing clinical trials in Australia. Blinatumomab is a BiTE that enables an immunological response between the CD19 positive leukaemic cell and a cytotoxic CD3 positive T-cell.
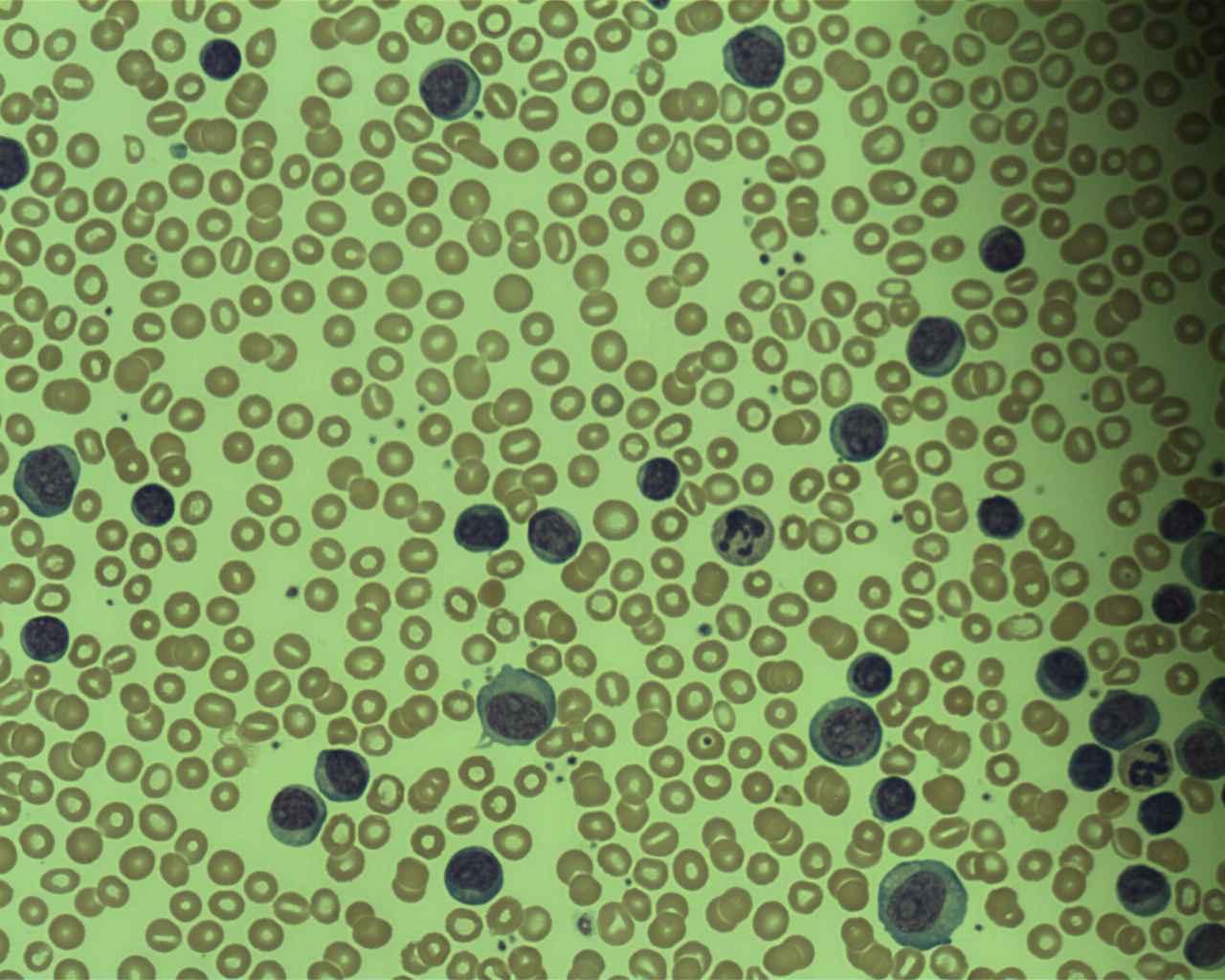
Lymphoblasts in Acute Lymphoblastic Leukaemia
Prof. Osaro Erhabor (CC BY-SA 4.0)
While the introduction of blinatumomab promises to be an exciting addition to the clinical arsenal, initial response rates in relapsed/refractory ALL have been ~43% and, as with other treatments, resistance is likely to occur. Immune evasion is a likely cause of resistance as well as loss of the CD19 target, leading to CD19 negative relapse and further investigation is warranted.
Relapsed patient samples that are identified as being treated with blinatumomab will be flow sorted by CD19 positivity. CD19 positive and CD19 negative populations will undergo mRNAseq to identify if a lineage switch has occurred and if the driving event is now present in the CD19 negative population. Differences in gene expression will also be interrogated.
Resistance will be modelled in-vitro by subjecting fusion constructs to incrementally increasing doses of blinatumomab, enabling further examination of potential immune evasion pathways.
Join our cancer research program
Acute Lymphoblastic Leukaemia (ALL) is the most common childhood cancer, and leading cause of non-traumatic death in children. For adolescents and young adults (AYA) with ALL the therapeutic outcomes are poor. Most older adults will die of their disease.
The recent wealth of genomic information has seen the emergence of new lesions known to confer high-risk, and other recurrent fusions and gene deletions for which the biological and clinical implications remain unclear.
Further, recent studies have implicated the human microbiome in ALL development, treatment response and life-long comorbidities. The major challenge is to incorporate knowledge gained through Next Generation Sequencing (NGS) into clinical care and to systematically identify druggable targets and rational effective therapies to improve patient outcomes.
To add to the complexity of therapeutic choice in ALL, immunotherapies (bi-specific T-cell engagers (BiTEs) and CAR-T cells), have shown efficacy in the relapsed/refractory setting, as a transplantation bridge. However, not all high-risk/relapsed ALL patients are eligible for immunotherapy, ~50% of patients experience severe hypersensitivity reactions and the long-term clinical sequelae remains unknown.
Our laboratory is the National Referral Centre for genomic screening of ALL cases across all age groups, as such we sequence a large number of patients and have identified a significant number of alterations and novel gene fusions for investigation.

Supervisors
Co-supervisors: Dr Sue Heatley
Research area: Cancer program - South Australian Health and Medical Research Institute
Recommended honours enrolment: Honours in Molecular and Biomedical Science
