From the lab bench to the clinic: Pneumonia vaccine shows commercialisation strengths
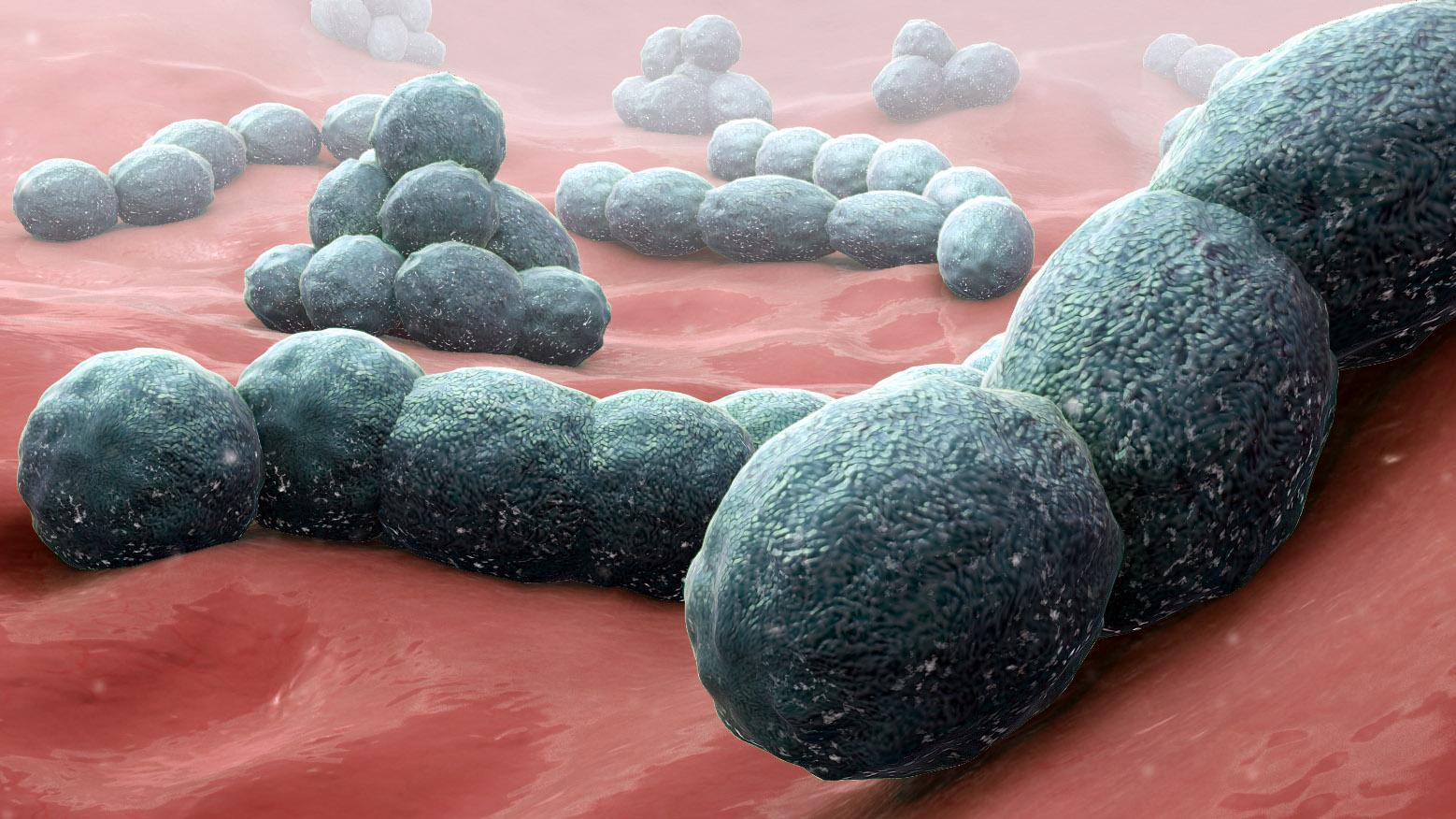
Image: Streptococcus pneumoniae bacteria, Manu5
Commercialisation potential of Faculty of Sciences’ research is in the spotlight after the development of a new Pneumonia vaccine.
Last month we reported that the University of Adelaide’s Research Centre for Infectious Diseases (RCID) were a step closer to a vaccine against the biggest bacterial killer on the planet, with funding secured for preclinical trials.
Led by Professor James Paton, the RCID team have been working on a vaccine for Streptococcus pneumoniae (the pneumococcus) that could save up to two million lives globally a year. The research also addresses the overuse of antibiotics that leads to resistance.
State MP Richard Harvey, Member for Newland, spoke in the House of Assembly last week about the new vaccine, and put a spotlight on this University of Adelaide research that had “made its way from the lab bench to the clinic”.
“This is one of many examples where Adelaide-based research is making exciting discoveries that drive investment from interstate and overseas into South Australia, by both leveraging funding from the federal government in the early stages and also, significantly, from private sources,” he said.
“State government support is playing an important role in helping to leverage such funding.”
As a scientist himself, Dr Harvey’s not a newcomer to the subject of Streptococcus pneumoniae. He worked with the RCID for more than 11 years and graduated with three science degrees from the University of Adelaide.
“Success such as this does a great deal to generate local research jobs in the short term and many more downstream high-skill opportunities for South Australians into the future as projects progress,” Dr Harvey said.
“Importantly, this demonstrates to students studying science in South Australia that there is a future for us, a career in science in South Australia, and that students studying science here for a career can indeed have a very real impact and address problems that impact millions of people around the world.”
Read Dr Harvey's speech below.
Full transcript
Tuesday 26 February
House of Representatives – Grievance Debate
Vaccine Development
Dr HARVEY (Newland): Today, I would like to talk about some recent local success in an area dear to my heart—that is, science. There is often a narrative in South Australia, and indeed Australia as a whole, that we are very good at basic fundamental research and discovering things but not as good at commercialising that research into something that can be produced and sold. To a certain extent, this is true, and there is work for us to do in this area.
It is worth noting that, on the state government's part, the Marshall government's Research, Commercialisation and Startup Fund will help address some of this issue and provide a local leg-up to projects reaching the early commercialisation phase. However, it is also worth noting that there are some great examples of where local research has successfully—and certainly in the case of medical research and not exclusively—made its way from the lab bench to the clinic.
A particular example I would like to talk about today has gained some local media attention and comes from my former workplace in the Research Centre for Infectious Diseases at the University of Adelaide under the leadership of Professor James Paton. This project has progressed to quite an advanced stage in the design of a new vaccine to protect against pneumococcal disease. Pneumococcal disease is responsible for more than one million deaths in children under five around the world.
Pneumonia, which is one of the leading diseases caused by this pathogen, is a leading cause of death in children worldwide. However, in addition to that, this bug is also responsible for very serious invasive diseases that can kill very quickly, and it is also responsible for the socially and economically debilitating condition otitis media, which is also known as ear infections. In Australia, this is particularly a concern in Indigenous Australian communities.
Currently, there are two vaccines used within Australia. There is a 23-valent or 23-type vaccine that is used in elderly people, and then there is a 13-valent vaccine used for children. These are effective for those types that are included in the vaccine, and these tend to be the most common types. But, given that there are almost 100 different types of this bug, the future will very likely require a vaccine that is able to cover all types of this bacterium. The project I am describing here today is working on a vaccine that would or could in the end protect against all types of pneumococcus.
This work started off at the fundamental stage looking at components on the surface of this bug that are present in all types of the bug and testing for their ability to protect against pneumococcal disease in in vivo models of disease. In concert with work looking at producing a vaccine that would protect against all strains of the flu, a similar kind of technology looked at using gamma irradiation to inactivate these bugs and then using that as a whole cell vaccine, which was then tested for the ability to provide protection in in vivo models of disease.
As a consequence, almost 18 months ago, Adelaide-based GPN Vaccines Proprietary Limited was created to develop this whole cell vaccine. The current chairman and CEO of that company is Dr Tim Hirst. Much of this work to this point was supported by a linkage grant from the Australian Research Council and, later, a development grant from the National Health and Medical Research Council, as well as early commercialisation funding from the state government and some seed capital from angel investors.
More recently, though, through a series A capital raise, GPN Vaccines successfully raised $1.1 million from Australian and overseas investors, which will support pre-clinical work looking at toxicity as well as how to scale up a clinical-grade state for the manufacture of this vaccine. This is a critical first step before further capital raising and likely other funding is required to support phase 1 human clinical trials to look at the safety and, basically, the ability to provide protection in humans.
This is one of many examples where Adelaide-based research is making exciting discoveries that drive investment from interstate and overseas into South Australia, by both leveraging funding from the federal government in the early stages and also, significantly, from private sources. State government support is playing an important role in helping to leverage such funding.
Success such as this does a great deal to generate local research jobs in the short term and many more downstream high-skill opportunities for South Australians into the future as projects progress. Importantly, this demonstrates to students studying science in South Australia that there is a future for us, a career in science in South Australia, and that students studying science here for a career can indeed have a very real impact and address problems that impact millions of people around the world.
