Cloning acute lymphoblastic leukaemia fusion genes and variants
Functional characterisation and therapeutic responses
Recent advances in genomic profiling have defined B-cell Acute Lymphoblastic Leukeamia (B-ALL) as a heterogeneous disease with multiple subgroups characterised by distinct genetic alterations. Many genomic lesions in B-ALL are associated with alterations of cytokine receptors or their signaling pathway mediators, transcription factors or regulators of differentiation.
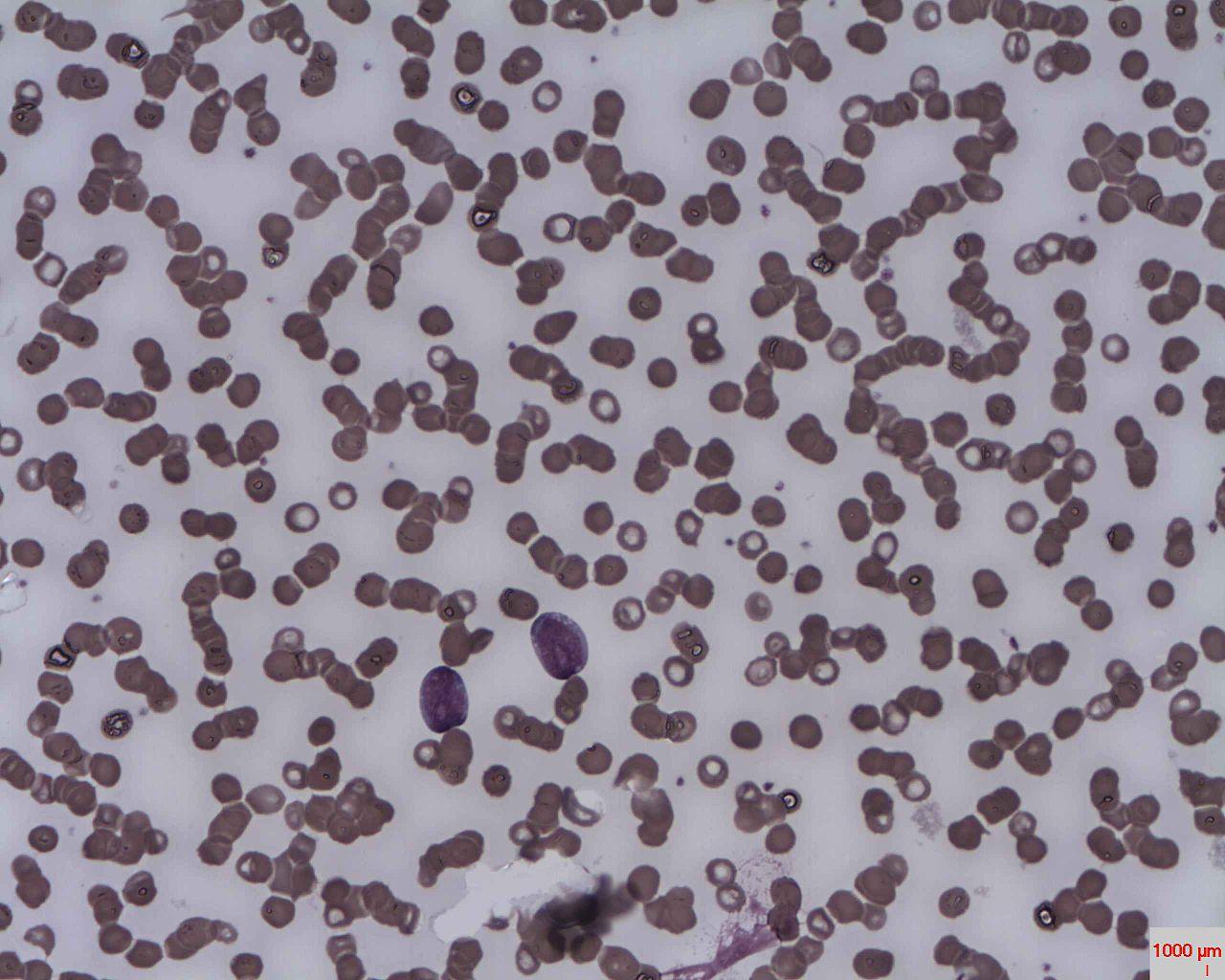
Acute lymphoblastic leukaemia
Dr Erhabor Osaro (CC BY-SA 3.0)
Genomic lesions in ALL patients stratify with prognosis and using transcriptomic analysis, we have identified a number of poorly characterised fusion genes and variants in patients.
This project aims to clone full-length fusion-genes and gene variants from patient material into mammalian expression plasmids. This will allow in vitro characterisation in cell line models of aberrant signalling pathways that drive disease and assess therapeutic responses.
This project will involve a range of molecular biology and cloning techniques including primer design, PCR Sanger sequencing, bacterial work, tissue culture and flow cytometry.
Join our cancer research program
Acute Lymphoblastic Leukaemia (ALL) is the most common childhood cancer, and leading cause of non-traumatic death in children. For adolescents and young adults (AYA) with ALL the therapeutic outcomes are poor. Most older adults will die of their disease.
The recent wealth of genomic information has seen the emergence of new lesions known to confer high-risk, and other recurrent fusions and gene deletions for which the biological and clinical implications remain unclear.
Further, recent studies have implicated the human microbiome in ALL development, treatment response and life-long comorbidities. The major challenge is to incorporate knowledge gained through Next Generation Sequencing (NGS) into clinical care and to systematically identify druggable targets and rational effective therapies to improve patient outcomes.
To add to the complexity of therapeutic choice in ALL, immunotherapies (bi-specific T-cell engagers (BiTEs) and CAR-T cells), have shown efficacy in the relapsed/refractory setting, as a transplantation bridge. However, not all high-risk/relapsed ALL patients are eligible for immunotherapy, ~50% of patients experience severe hypersensitivity reactions and the long-term clinical sequelae remains unknown.
Our laboratory is the National Referral Centre for genomic screening of ALL cases across all age groups, as such we sequence a large number of patients and have identified a significant number of alterations and novel gene fusions for investigation.

Supervisors
Co-supervisors: Dr Barbara McClure
Research area: Cancer program - South Australian Health and Medical Research Institute
Recommended honours enrolment: Honours in Molecular and Biomedical Science
